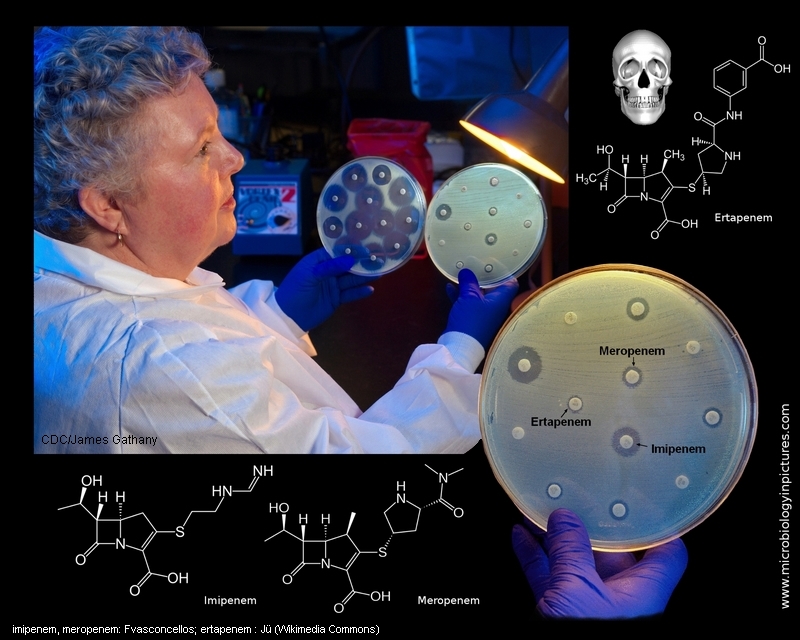
This image depicts Centers for Disease Control (CDC) microbiologist Kitty Anderson holding up two Petri dish culture plates growing bacteria
in the presence of discs containing various antibiotics. The isolate, i.e., bacterial specie, on the left plate is susceptible to the antibiotics on the discs, and is therefore, unable to grow adjacent to
the discs. The plate on the right was inoculated with a Carbapenem-Resistant Enterobacteriaceae (CRE) bacterium that proved to be resistant to almost all of the antibiotics tested, and is
therefore, able to grow near the discs.
CRE are a family of germs that are difficult to treat because they have high levels of resistance to antibiotics. Klebsiella species and Escherichia coli are examples of Enterobacteriaceae, a normal part of the human gut bacteria, that can become carbapenem-resistant.
About carbapenems:
Carbapenems are a class of β-Lactam antibiotics with a broad spectrum of antibacterial activity. They have a structure that renders them highly resistant to most β-lactamases. Carbapenem antibiotics were originally developed from the carbapenem thienamycin, a naturally derived product of Streptomyces cattleya.
Carbapenems are one of the antibiotics of last resort for many bacterial infections, such as Escherichia coli (E. coli) and Klebsiella pneumoniae. Recently, alarm has been raised over the spread of drug resistance to carbapenem antibiotics among these coliforms, due to production of carbapenemases, including the New Delhi metallo-β-lactamase, NDM-1. There are currently no new antibiotics in development to combat bacteria resistant to carbapenems, and worldwide spread of the resistance gene is considered a potential nightmare scenario.
