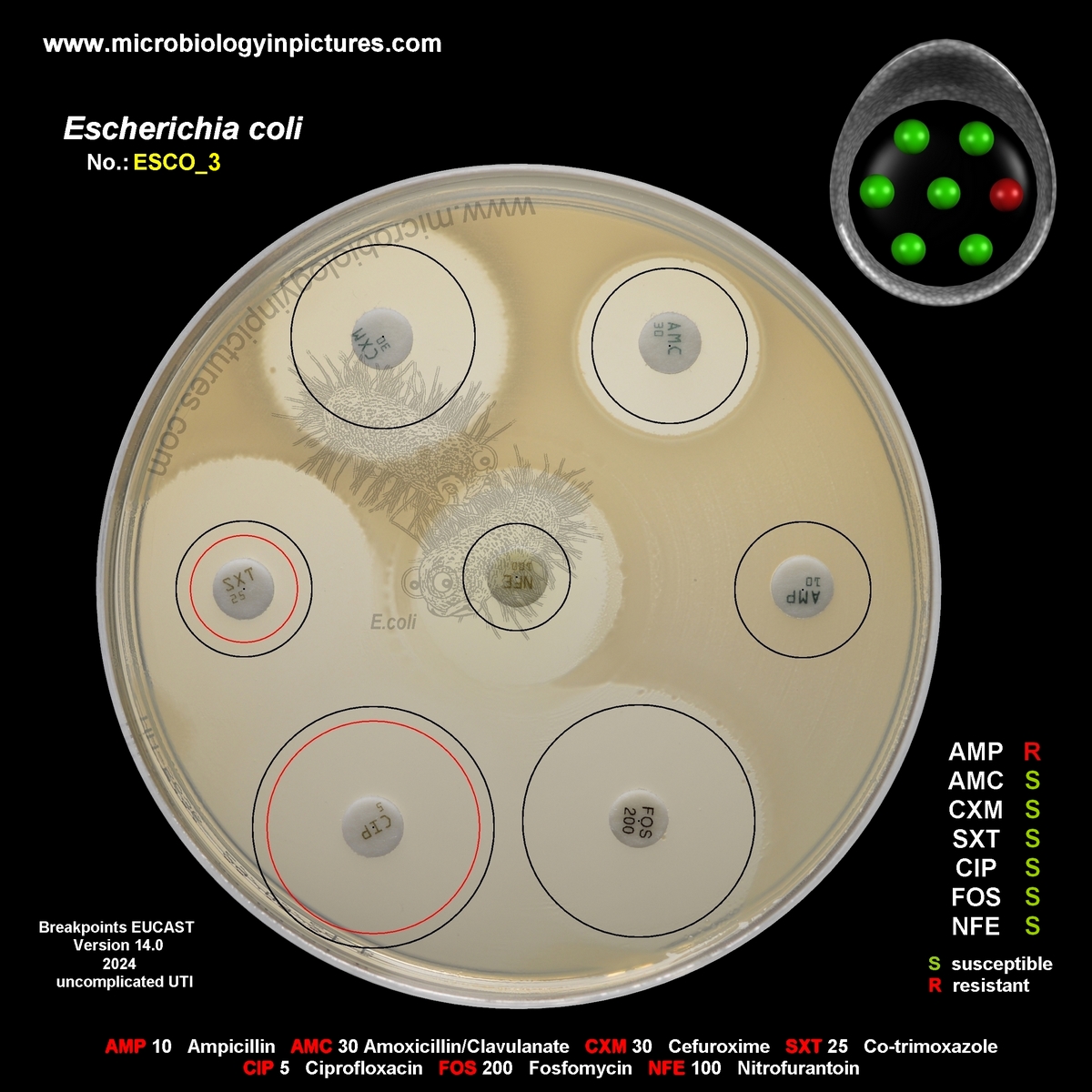
Escherichia coli resistant to ampicillin. Beta-lactam antibiotics.
Seven antibiotic disks are placed on the agar plate:
- 1. Ampicillin
- 2. Amoxicillin/Clavulanate
- 3. Cefuroxime
- 4. Co-trimoxazole
- 5. Ciprofloxacin
- 6. Fosfomycin
- 7. Nitrofurantoin
After overnight incubation, inhibition zones around the antibiotic disks are observed. An agar plate before overnight cultivation you can find here (fosfomycin replaced with gentamicin). There is no inhibition zone around the AMP 10 disk in the picture above (inhibition zone = 6 mm; diameter of the disks is 6.2 mm), indicating resistance to ampicillin.
Breakpoints for E.coli you can find here (EUCAST 2024)
Interpretation of the Results:
Ampicillin = Resistant
The strain shows resistance to ampicillin. This means that ampicillin will not be effective in treating the infection caused by this E. coli strain. Resistance to ampicillin in E. coli is often due to the production of beta-lactamases (enzymes that break down the beta-lactam ring of the antibiotic). This is a common form of resistance in clinical settings, especially in hospital-associated strains.
Ampicillin is a semi-synthetic penicillin antibiotic derived from penicillin G (discovered by Alexander Fleming in 1928). Ampicillin was developed in the 1960s by researchers at Beecham Group (now part of GlaxoSmithKline) as a broader-spectrum penicillin. It was designed to overcome some of the limitations of penicillin G (E.coli is intrinsically resistant to penicillin G), particularly its vulnerability to beta-lactamase enzymes produced by certain bacteria.
Mechanism of Action: Like other beta-lactam antibiotics, ampicillin works by inhibiting bacterial cell wall synthesis, leading to the death of the bacteria. It specifically targets the penicillin-binding proteins (PBPs) involved in the final steps of cell wall construction.
Ampicillin remains a key treatment for various bacterial infections in both hospital and community settings.
Amoxicillin/Clavulanate = Susceptible
The strain is susceptible to amoxicillin/clavulanate, which combines amoxicillin (a beta-lactam) with clavulanic acid (a beta-lactamase inhibitor). This combination can be effective against beta-lactamase-producing E. coli strains because clavulanate inhibits the beta-lactamases that break down amoxicillin.
Cefuroxime = Susceptible
The strain is susceptible to cefuroxime, a second-generation cephalosporin. This suggests that the E. coli strain does not produce extended-spectrum beta-lactamases (ESBLs) that would break down cefuroxime, and it can be used as a treatment option.
Co-trimoxazole = Susceptible
The strain is susceptible to co-trimoxazole (trimethoprim/sulfamethoxazole). It can be used as a treatment option.
Ciprofloxacin = Susceptible
The strain is susceptible to ciprofloxacin, a fluoroquinolone. This means the bacteria can be treated with ciprofloxacin (and other fluroquinolones), as it can penetrate the bacterial cells and inhibit DNA replication.
Fosfomycin = Susceptible
The strain is susceptible to fosfomycin, which is used to inhibit bacterial cell wall synthesis. This antibiotic is often used for urinary tract infections and would be effective in treating this strain.
Nitrofurantoin = Susceptible
The strain is susceptible to nitrofurantoin, which is effective primarily for urinary tract infections caused by E. coli. This suggests that nitrofurantoin could be a good choice for treating UTIs.
Implications for Antibiotic Selection
Based on the antibiotic susceptibility testing results, ampicillin should be avoided for the treatment of this E. coli infection, as the strain is resistant to it. However, amoxicillin/clavulanate, cefuroxime, co-trimoxazole, ciprofloxacin, fosfomycin, and nitrofurantoin all appear to be effective treatment options, depending on the location and severity of the infection. The selection of the best antibiotic should also take into account factors like the infection site (e.g., urinary tract, bloodstream), potential side effects, patient allergies, and local resistance patterns.
| AMP | Ampicillin | AMC | Amoxicillin/Clavulanate | CXM | Cefuroxime | SXT | Trimethoprim-Sulfamethoxazole |
| CIP | Ciprofloxacin | FOS | Fosfomycin | NFE | Nitrofurantoin |
Text generated with the help of OpenAI's language model, ChatGPT.
