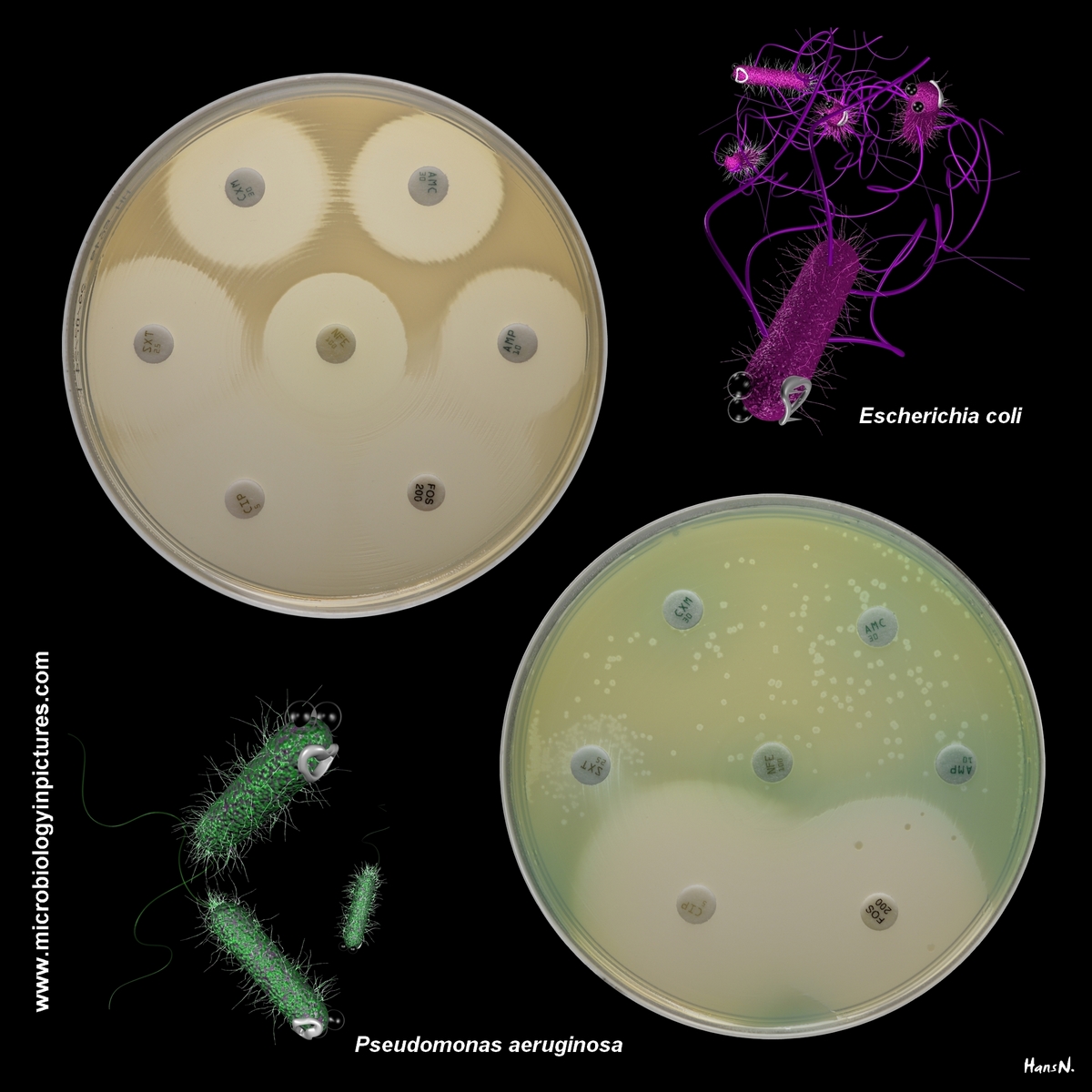
A good susceptible strain of Escherichia coli and a good susceptible strain of Pseudomonas aeruginosa.
Pseudomonas aeruginosa is not a common cause of UTIs in otherwise healthy individuals. It is more often associated with complicated or healthcare-associated UTIs. P.aeruginosa is known for its intrinsic resistance to several antibiotic classes and its ability to develop further resistance, making treatment challenging.
Studies suggest P.aeruginosa accounts for about 2-10% of UTIs overall, with much of this occurring in healthcare-associated or complicated cases.
A comparison of the listed antibiotics in terms of their effectiveness against infections caused by Escherichia coli and Pseudomonas aeruginosa:
Ampicillin (AMP)
Against E. coli: Limited effectiveness. Many strains of E. coli have developed resistance due to β-lactamase production.
Against P. aeruginosa: Ineffective. Pseudomonas aeruginosa is intrinsically resistant to ampicillin.
Amoxicillin/Clavulanate (AMC)
Against E. coli: Effective against many E. coli strains, particularly those producing β-lactamase enzymes. However, increasing resistance is observed in some regions.
Against P. aeruginosa: Ineffective. Pseudomonas aeruginosa is resistant due to intrinsic mechanisms and efflux pumps.
Cefuroxime (CXM)
Against E. coli: Effective for many E. coli infections, especially uncomplicated UTIs, though resistance is increasing due to extended-spectrum β-lactamases (ESBLs).
Against P. aeruginosa: Ineffective. Pseudomonas aeruginosa is intrinsically resistant to most 2nd-generation cephalosporins.
Trimethoprim/Sulfamethoxazole (SXT)
Against E. coli: Commonly used for E. coli infections, particularly uncomplicated UTIs. Resistance is a concern in some areas (ranging from 20–40% in certain regions).
Against P. aeruginosa: Ineffective. Pseudomonas aeruginosa is resistant to TMP-SMX.
Ciprofloxacin (CIP)
Against E. coli: Effective. Resistance is a growing issue due to widespread use.
Against P. aeruginosa: One of the most effective oral options. It is often used for Pseudomonas infections, but resistance can occur, particularly in healthcare settings.
Fosfomycin (FOS)
Against E. coli: Highly effective for uncomplicated E. coli UTIs, including many multidrug-resistant strains. Often used as a single-dose treatment.
Against P. aeruginosa: Limited effectiveness. Fosfomycin has some activity against Pseudomonas, but it is not a first-line option.
Nitrofurantoin (NFE)
Against E. coli: Highly effective for uncomplicated UTIs caused by E. coli. Limited activity in the bloodstream, so not suitable for systemic infections or pyelonephritis.
Against P. aeruginosa: Ineffective. Pseudomonas aeruginosa is intrinsically resistant to nitrofurantoin.
Text generated with the help of OpenAI's language model, ChatGPT.
21.12.2024
